
Editorial Note: We continue to feature Dr. Gregory Olson’s three part series on opioid prescription abuse. The third and final installment will be available Monday, June 6th.
For further information on help and treatment, please visit Substance Abuse and Mental Health Services Administration’s website (www.samhsa.gov/find-help)
Opioid Abuse Part 2: Crisis in Context
In my previous post, Opioid Abuse Part 1: Headlines and Policy, I discussed how renewed national attention toward opioid-drug abuse has pushed the issue to a top priority. Many by now have learned our nation is caught in the grips of an opioid addiction that is classified as an epidemic by the Centers for Disease Control and Prevention (CDC).
In this installment, I provide three windows for viewing the context surrounding opioid abuse. The first window provides an abbreviated overview of select mortality statistics (that is, number of deaths). The second describes a force behind the rise in opioid prescriptions. The final window profiles those most at risk for opioid abuse.
My intent is to stimulate deeper curiosity and thought about what is being reported and how we decide to focus policy decisions. Please engage in this discussion especially if you have first-hand knowledge of someone struggling with addiction to pain medication.
How Many Americans Are Dying and From What?
“DEA Releases New Drug Overdose Death Figures: Guns Safer than Prescription Drugs”1
“46,471: Drug Overdoses Killed More Americans Than Car Crashes or Guns.”2
These and many similar headlines use the number of drug overdose deaths to grab our attention and imply that some threshold of tolerance or acceptability has been crossed. But how do fatal drug overdoses and, more specifically, opioid deaths actually compare to other causes of death?
The table below compares deaths related to addictions and to other causes interesting from a policy perspective. As you review the data, keep in mind that the percent change from 2000 to 2013 is not corrected for changes in population size; the US population grew from 282.2 million in 2000 to 316.5 million in 2013, a 12.2% increase.3
Cause and number of deaths in 2000 and 2013
| Causes of Death | 20004 | 20135,6 | % Change |
|---|---|---|---|
| Total Reported from All Causes | 2,403,351 | 2,596,993 | +8.1 |
| Heart Disease (#1 Cause) | 710, 760 | 611,105 | -14 |
| Cigarette Related | >443,595 | >480,000 | +8.2 |
| Medical Error in Hospitals | 225,000** | 440,000 | +95.5 |
| Drug Induced (legal & illegal) | 19,698 | 46,471 | +135.9 |
| Second-Hand Smoke Related | 49,400 | 41,000 | -17 |
| Motor-Vehicle Related | 43,354 | 35,369 | -18.4 |
| Firearm-Related | 28,663 | 33,636 | +17.3 |
| Alcohol Induced* | 19,358 | 29,001 | +49.8 |
| Prescription-Opioid Induced | 4,000 | 18,893*** | +372.3 |
*Alcohol-related deaths were approximately 88,000 for 2013.
**Number quoted is the lowest from reported estimates.
***From 2014 data
The numbers above show that while more people die from drugs than from cars or guns, fewer die specifically from prescription opioids. Perhaps it is the dramatic rate increase in opioid deaths that raises alarm. This incredible leap of 372% parallels the rise in the number of prescriptions for opioids. Both news headlines and policymakers have pointed to the relation between these two sobering trends.
As an aside, it may be tempting to speculate that the higher number of car- and gun-related deaths is due to a significantly higher volume of cars and guns in our country. In 2012, the CDC reported that 259 million opioid pain-relief prescriptions were written. Coincidentally, the US Department of Transportation estimated in 2013 that 255.8 million registered passenger cars were on the road. The number of registered and unregistered firearms in the US is estimated to be between 270 and 310 million. As you can see, the total number of cars and guns are surprisingly comparable to the number of opioid prescriptions.
While the quantity of vehicles, firearms and opioid prescriptions doesn’t tell the whole story, it does appear to have some relationship to adverse outcomes. Given this, curbing the number of opioid prescriptions should be a worthwhile pursuit. What explains the recent explosion in opioid prescriptions? Is the increased number contributing to addiction or merely responding to addiction?
Big Data, Super Salesmen and Susceptibility
In 1996, Purdue Pharma introduced OxyContin, an opioid pain drug, to the market. The distribution of this pain drug expanded rapidly due to aggressive and innovative sales strategies attributed to one of the owners who was also a psychiatrist and advertising guru. These marketing strategies included:
- Fostering relationships with doctors
- Compiling data on prescribing habits, then targeting frequent prescribers for increased sales attention
- Targeting additional indications for drug use
- Obtaining repeated FDA approval of higher single-dosage pills
- Aggressively promoting OxyContin as a “safe alternative” to other opioids, with a “low potential for addiction, <1%”7
The combined sales and repackaging efforts contributed to OxyContin earning almost 30% of the market share and more than $3 billion in annual profits. Those who manage pain appropriately agree that opioids have their place as effective analgesics in the spectrum of pain management. The concern here is that safety and efficacy may have fallen secondary to profit.
At-Risk Individuals and Regions
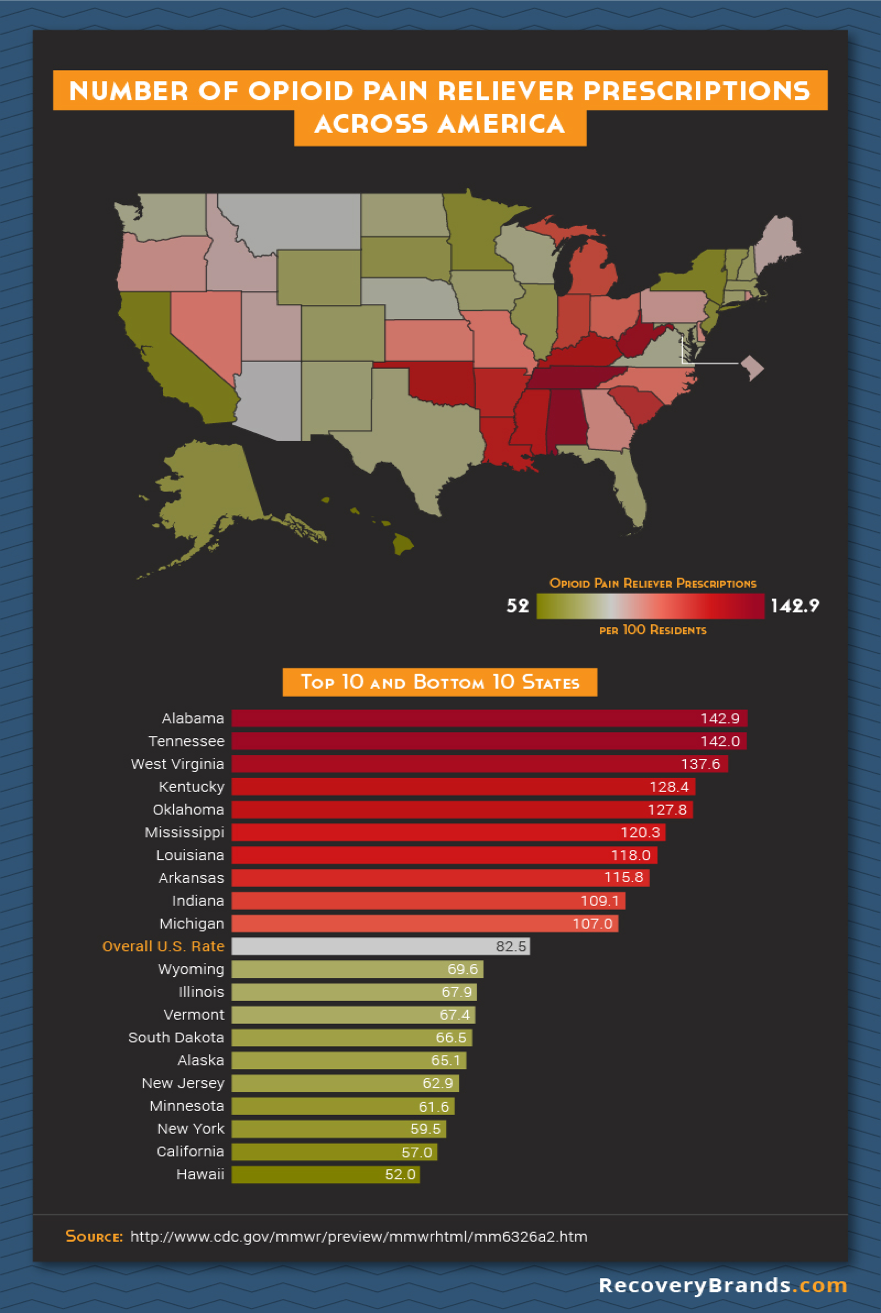
By now it’s clear that prescription rates have grown exponentially in part due to demand, sales tactics and the willingness to prescribe. This growth has not been uniform across the country, however. The marketing strategy of identifying clinics and physicians who were writing the most pain prescriptions likely created considerable regional variation in opioid use (refer to map).
The profile of individuals experiencing the most prescription opioid overdoses seems to reflect this regional variation but is different than what the media has led us to expect.
Profile of an Individual Most at Risk for Opioid Painkiller Abuse:8
- Male
- Between the ages of 45-55
- Caucasian (predominantly) or Native American
- History of substance abuse, mental illness, chronic pain
- Non-urban
- Has multiple filled prescriptions from numerous providers
- High daily dose
- Low income/receives Medicaid
Lessons Learned?
The data and context we’ve reviewed thus far suggest that our protective processes are slow and typically reactive rather than proactive. We treat diseases and leave health to emerge on its own. I wonder if our national consciousness is able to focus on only a limited number of topics at a time and thus is prone to wander from one to another as urgency dictates.
Substance abuse and addiction have a vibrantly-consistent history in the US. Times of plenty and times of stress both feed the general patterns. What have we learned? What haven’t we learned? When will evidence-based practice prevail in prevention and treatment?
In spite of policy-enforced efforts, the numbers of car-, gun-, cigarette- and alcohol-related deaths persist at an unacceptable rate. Can we make opioid policies more effective? Is this problem more rapidly solvable? Are the contributing factors different in some more changeable way?
As the United States struggles to keep up with the health care demands of a growing population, limited resources force us to make practical and ethical choices. Examining the context for opioid abuse can inform how we set public policy and reveal our attitudes toward population and individual health.
In the next installment, I will discuss current action plans and offer some upstream options that might begin the shift from a culture of treating disease to a culture of health.
Gregory Olson, DDS, MS
Gregory Olson, DDS, MS, is a board certified pediatric dentist and orthodontist. He is currently an associate professor at Loma Linda University School of Dentistry and also a Faculty Scholar for the Institute for Health Policy and Leadership.
Dr. Olson has recently completed the Harry W. Bruce Jr. Legislative Fellowship with the American Dental Education Association and now serves on their Legislative Advisory Council. He is committed to investing in innovative partnerships, ideas and policies that will improve the health and well-being of all.
For more information contact Dr. Gregory Olson at: golson@llu.edu.
- Accessed May 13, 2016: https://mises.org/blog/dea-releases-new-drug-overdose-death-figures-guns-safer-prescription-drugs
- Accessed May 13: 2016: http://www.cnsnews.com/news/article/susan-jones/dea-drug-overdoses-kill-more-americans-car-crashes-or-firearms
- Accessed April 28, 2016: http://www.census.gov/popclock/
- Accessed April 28, 2016: http://www.cdc.gov/nchs/data/nvsr/nvsr50/nvsr50_16.pdf
- Accessed April 28, 2016: http://www.cdc.gov/nchs/fastats/deaths.htm
- Accessed April 28, 2016: https://www.nhtsa.gov/research-data/fatality-analysis-reporting-system-fars
- Accessed May 18, 2016: http://theweek.com/articles/541564/how-american-opiate-epidemic-started-by-pharmaceutical-company
- Accessed April 28, 2016: Vital Signs: Demographic and Substance Use Trends Among Heroin Users — United States, 2002–2013 http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6426a3.htm
Did you like this article? We want to hear from you! Leave your comments or questions in the space below.
Please note that the views expressed in this article do not necessarily represent those of Loma Linda University Health or the Institute for Health Policy and Leadership.

