
Infertility affects individuals and couples across the world,1 and access to infertility treatment varies widely across countries, influenced by healthcare systems, culture, and economic factors. 2 In many European countries like France, Germany, and the UK, treatments such as in vitro fertilization (IVF) are publicly funded. 3 Australia also subsidizes fertility care through Medicare,4 while Japan began fully covering assisted reproductive technologies in 2022 in response to its declining birthrate. 5 In contrast, in the U.S., most infertility care is not federally mandated.6 IVF can cost up to $25,000 per cycle, often paid out of pocket. 7
According to the Centers for Disease Control’s National Survey of Family Growth (2015–2019), approximately 13.4% of women and 11.4% of men aged 15–49 experience infertility.8 Despite this prevalence, access to assisted conception methods such as intrauterine insemination (IUI) and in vitro fertilization (IVF) remains uneven, largely shaped by insurance policies and state-level regulations. According to a recent publication, 21 states—including California, Texas, New York, Massachusetts, Illinois, and Maryland—mandate some level of infertility insurance coverage.6
California has since taken significant steps to expand access. Under Senate Bill 729 (SB 729), starting January 1, 2026, large group health insurance policies covering more than 100 employees must provide comprehensive coverage for infertility diagnosis and treatment. Importantly, it also strengthens non-discrimination protections. Health plans may not impose different terms, conditions, or limitations based on age, sex, gender identity, sexual orientation, marital status, or other protected characteristics.9
Despite these legislative efforts, IVF continues to be a topic of complex societal discussion in the U.S. Ethical debates persist regarding issues such as embryo selection, storage, and equitable access based on personal characteristics.10 Additionally, religious and political perspectives play a significant role in shaping state-level policies, which contribute to ongoing disparities in coverage and access.11
Public opinion on IVF in the U.S. is generally supportive, particularly as infertility becomes more openly discussed and understood as a medical condition. Many Americans view assisted reproductive technologies as essential for helping individuals and couples build families.
A national survey conducted by Verasight offers insights into how personal experiences with infertility influence public opinion on these critical healthcare issues. With responses from 1,000 Americans, Verasight explored two primary questions:
- To what extent do people support a law requiring health insurance to cover assisted conception methods such as IUI or IVF?
- Do people support the rights of infertility patients to pursue IVF treatments without restrictions?
The results show a clear trend: proximity to infertility, whether through personal, family, or friends, strongly correlates with support for both insurance coverage and IVF rights.
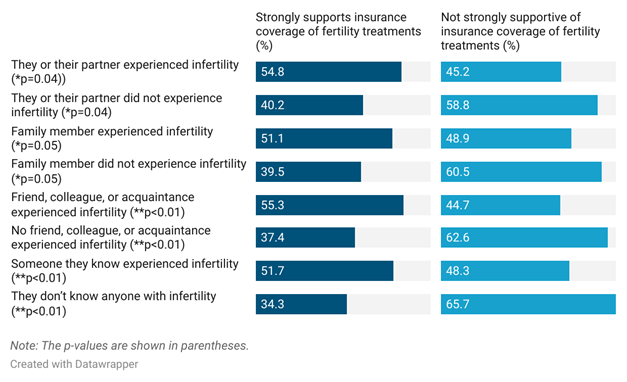
Infertility Experience Elevates Support for Insurance Coverage
Figure 1 shows that respondents who had personally experienced infertility (either themselves or through a partner) strongly support law requiring insurance coverage for assisted conception treatments (54.8%). In contrast, only 40.2% of those without personal experience expressed strong support.
Support also increased with indirect exposure. If a family member experienced infertility or they knew a friend, colleague, or acquaintance with infertility, they strongly support coverage (51.1% and 55.3%, respectively), compared to people without that connection (39.5% and 37.4%, respectively).
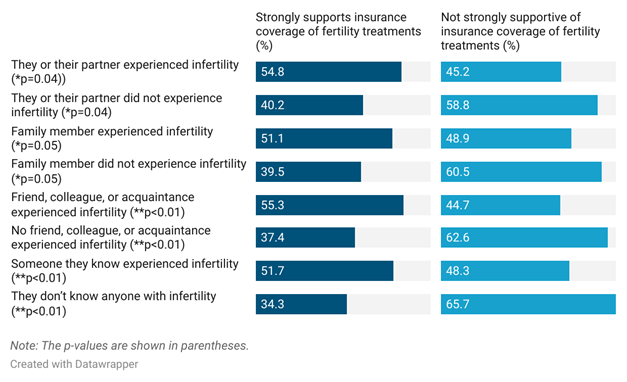
Figure 1. Respondent responses when asked about their experiences with infertility and support for a law requiring health insurance companies to cover assisted conception methods.
Support for IVF Rights Also Linked to Personal Connection
The trend continues when examining support for the right to unrestricted access to IVF (see Figure 2). Individuals with personal or a partner’s infertility experience were more likely (66.7%) to support IVF without restrictions than people without those experiences (54.8%). Having a family member affected (59.3%) or knowing a colleague who experienced infertility (67.2%) also increased support, compared to those without these social ties.
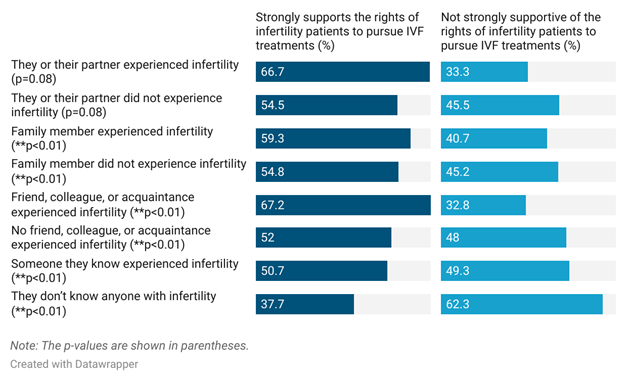
Figure 2. Respondent responses when asked about their experiences with infertility and support for the rights of infertility patients to pursue IVF treatments.
Key Takeaways: Personal Relevance Drives Policy Preferences
According to the Verasight data, people are more likely to support reproductive health rights and coverage when they experience infertility firsthand or through someone they know. However, even among those without experience, a sizable portion of respondents still support a more empathetic and inclusive future for fertility treatments.
This reinforces the need for:
- Public education campaigns to raise awareness about infertility,
- Policy advocacy to push for inclusive insurance coverage,
- And continued research into how social networks and lived experiences shape health policy attitudes.
Co-Author Bios

Safiye Sahin, PhD, RN
Dr. Safiye Sahin is a researcher at the Loma Linda University School of Nursing, specializing in health policy, nursing management, and public health nursing. Her research centers on family-friendly benefits, health policies, and access to care for individuals with sickle cell disease. She employs mixed methods, qualitative inquiry, and evidence synthesis to develop culturally responsive and community based interventions. With over a decade of academic teaching and research experience, she is committed to contributing to efforts that promote quality in healthcare systems.

Lisa R. Roberts, DrPH, MSN, FNP-BC, FAAN, FAANP
Dr. Roberts is a Professor and the Research Director at the School of Nursing, with a secondary appointment in the Division of Interdisciplinary Studies in the School of Behavioral Health. She is a Fellow of the American Association of Nurse Practitioners and the American Academy of Nursing. Her primary research interest concerns maternal health and sickle cell disease. Her research interests also include mixed methods and community-based self-help interventions, addressing issues impacting health disparities and vulnerable populations. Her clinical focus as a Family Nurse Practitioner is prevention and primary care.
References:
- World Health Organization (WHO). Infertility prevalence estimates, 1990–2021: World Health Organization; 2023. Retrieved from: https://www.who.int/publications/i/item/978920068315
- Mackay A, Taylor S, Glass B. Inequity of access: scoping the barriers to assisted reproductive technologies. Pharmacy. 2023;11(1):17.
- Reproduction EI-MCftESoH, Embryology, Calhaz-Jorge C, Smeenk J, Wyns C, De Neubourg D, et al. Survey on ART and IUI: legislation, regulation, funding, and registries in European countries—an update. Human Reproduction. 2024;39(9):1909-24.
- Adamson GD, Cheong Y, Fatemi H, Ferriani R, Griesinger G, Pellicer A, et al. Policy solutions to improve access to fertility treatment and optimise patient care: Consensus from an expert forum. 2024. [Available from: https://www.commonwealthfund.org/publications/scorecard/2024/jul/2024-state-scorecard-womens-health-and-reproductive-care
- https://www.organon.com/wp-content/uploads/sites/2/2024/07/Access-to-fertility-treatment-white-paper-CRA-Organon-rev-07-01-24.pdf
- Katagiri Y, Jwa SC, Kuwahara A, Iwasa T, Ono M, Kato K, et al. Assisted reproductive technology in Japan: a summary report for 2022 by the Ethics Committee of the Japan Society of Obstetrics and Gynecology. Reproductive Medicine and Biology. 2024;23(1):e12620.
- Popovic A, Jain K, Gillan E, Pandher M, Alwaal A. State Laws and Insurance Coverage for Male Infertility. Urology. 2025 Jun;200:91-96. doi: 10.1016/j.urology.2025.03.025. Epub 2025 Mar 18. PMID: 40113148.
- Peipert BJ, Mebane S, Edmonds M, Watch L, Jain T. Economics of fertility care. Obstetrics and Gynecology Clinics. 2023;50(4):721-34.
- Nugent CN, Chandra A. Infertility and impaired fecundity in women and men in the United States, 2015–2019. National Health Statistics Reports, 2024 Apr;(202):1-19. PMID: 38722687.https://ihpl.llu.edu/sites/ihpl.llu.edu/files/2025-07/July_2025_PB.pdf
- Institute for Health Policy and Leadership. Policy At A Glance: Health Care Coverage: Treatment for Infertility and Fertility Services (SB 729): Loma Linda University; July 2025 Retrieved from:
- Cohen IG, Adashi EY. Ethical and legal implications of in vitro gametogenesis and germline editing—current status. Fertility and Sterility. 2025;124(1):30-6.
- Wittenburg, K. M. (2025). Exploring religious leaders’ perspectives on genetic counseling, testing, and related technologies (Order No. 31846039). Available from ProQuest Dissertations & Theses Global. (3190907785). Retrieved from https://www.proquest.com/dissertations-theses/exploring-religious-leaders-perspectives-on/docview/3190907785/se-2
