Breast cancer is the most common cancer diagnosis and second leading cause of cancer death in women in the United States. Early detection is key to improving cancer survival and minimizing harms of treatment. Under existing California state law and the Affordable Care Act, screening mammograms must be covered by insurers without out of pocket costs to patients. However, any additional follow up or diagnostic testing may not be covered. If a woman cannot afford the cost of diagnostic testing, then she may delay treatment and have a worse outcome from her cancer. California Senate Bill 974, which was introduced on February 10, 2022, and passed by the Senate on May 25, requires health insurers to cover diagnostic and supplemental screening breast imaging in addition to screening mammograms without cost sharing.1
Under current state and federal laws, screening mammograms are a preventive service covered by insurers and cannot result in requiring a patient to pay a copay. Diagnostic and supplemental screening breast imaging differ from screening breast imaging. Screening breast imaging is used when a healthy person without any breast problems undergoes a mammogram, which is an x-ray of their breast, to detect early signs of cancer. When someone is found to have an abnormality on a screening mammogram, they have to come back for diagnostic breast imaging of the breast that was found to have the problem. If someone is found to have a lump in their breast, they will also require diagnostic breast imaging. For healthy people who are born with a breast cancer gene that predisposes them to developing breast cancer, supplemental screening breast imaging is required more frequently to detect cancer early. Diagnostic and supplemental breast imaging most commonly include additional magnified or three dimensional mammograms, ultrasounds, or breast MRI. These imaging studies are required to follow up any abnormalities found on screening and have been shown to increase detection rates in high risk individuals.
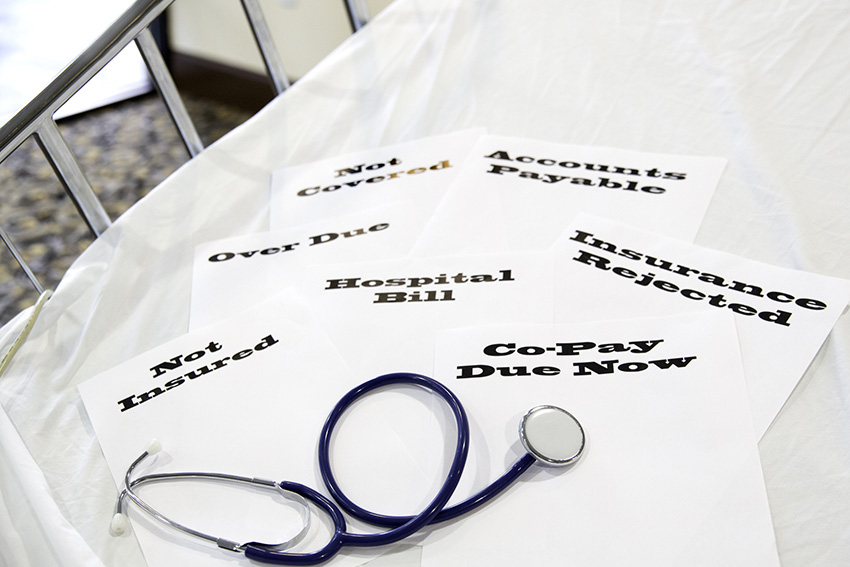
Presently, if someone needs additional breast imaging because they found a lump, they are at high risk for getting breast cancer, or they were found to have an abnormal screening mammogram, they may be required to pay out of pocket to receive these services. The average price a patient would have to pay for an additional mammogram is $143.98; for breast MRI, $342.60; for breast ultrasound, $113.15; for 3D mammogram, $51.07; and for related biopsies, $185.88.2 Studies have shown that cost sharing is associated with decreased patient compliance. Financial burden is a barrier to care associated with disparities in care that leads to inequitable health outcomes. While the current law helps to provide access to screening mammograms, the ability to detect and treat breast cancer early, in a curable stage, is inadequate without requiring coverage of diagnostic and supplemental screening breast imaging.
SB 974 provides an amendment to the current requirement for screening mammogram coverage in California. For those enrolling in covered plans starting in January 2023, this bill would prohibit cost-sharing for all medically necessary breast imaging for 1) women 40-74 years who need it for diagnostic screening when average risk or for supplemental screening when at increased risk; 2) men and women at increased risk for breast cancer who need it for diagnostic or supplemental screening purposes; and 3) men and women at average risk requiring diagnostic imaging.1 This bill would cover 22.8 million Californians, of whom 65% currently have some cost sharing requirement for these services. Approximately 942,908 covered individuals have breast imaging each year and utilization is expected to increase by 4.1% with passage of this bill.2 While net annual expenditures are estimated to be $43,742,000, the difference in excess treatment costs between treating a cancer that is 2 cm in size due to a delay in care compared to one that is 1 cm in size treated early could equate to as much as $550,000 per patient.3,4 This excess cost of treatment is attributed to the added expenses of combination chemotherapy and targeted therapy, mastectomy, and reconstruction—all of which could potentially be avoided if a patient can treat her breast cancer early.
In summary, SB 974 fixes a loophole in existing California law that will prevent women from developing late stage cancers that require them to lose their breasts and need chemotherapy and will prevent exacerbating disparities in care by mitigating financial toxicity. As the bill has passed out of the Senate and is currently being considered in the CA Assembly, it has not become law yet. The hope is that it will be soon.
Author Bio
Sharon Lum, MD, MBA, FACS
Dr. Lum is Professor and Chair of the Department of Surgery for the School of Medicine. She is a member of the American Society of Breast Surgeons Health Disparities Advisory Committee. Her research interests include quality measures and disparities in breast and other cancer outcomes and incorporation of patient reported outcomes in clinical decision-making for patients with breast diseases.
References
- https://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=202120220SB974
- http://analyses.chbrp.com/document/view.php?id=1672
- Berlin NL, Chung KC, Matros E, Chen JS, Momoh AO. The Costs of Breast Reconstruction and Implications for Episode-Based Bundled Payment Models. Plast Reconstr Surg. 2020;146(6):721e-730e.
- https://www.practiceupdate.com/content/with-perjeta-the-cost-of-her2-breast-cancer-therapy-goes-up/12388
