
Part 3 of Addressing the Organ Shortage Crises in America: Fixing the Inequalities in Organ Distribution Policies
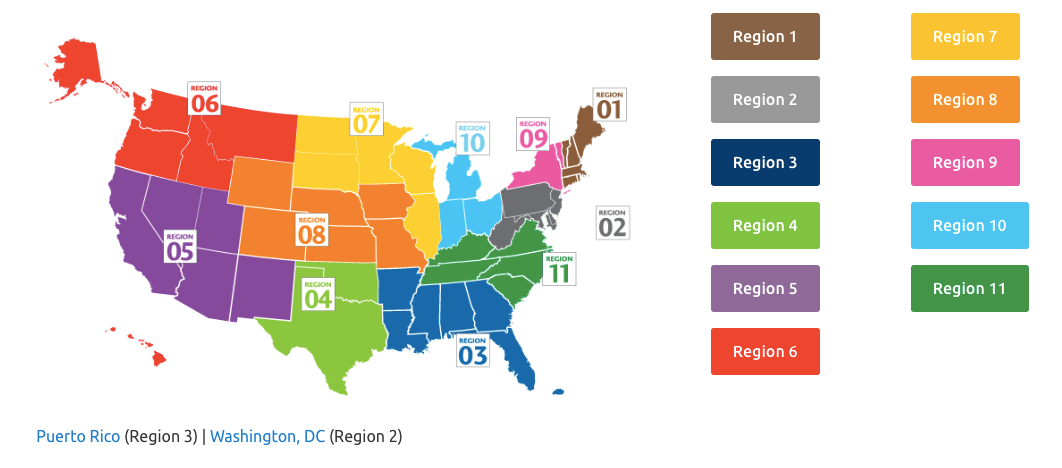
As we learned in the first part of this series, 20 people in the United States die every day waiting for a transplant.1 The organ allocation system has many disparities stemming from various causes. For one, geographic delineations result in disparities in distribution. The system is split into 11 regions, each encompassing a few bordering states (see map below).2 Until recently, the policies remained more or less unchanged since the early 2000s and a person’s chance of receiving an organ was heavily based on where they lived with some regions having a much smaller demand and higher supply. The laws necessitated that the organ must first go to patients within the region and local areas.3 That meant that sicker patients who were further away were less likely to have access to the organs than people who were less sick but closer.4 State policies such as stricter helmet laws can affect supply and demand, as can the demographics of an area.5 For instance, regions with a higher proportion of immigrants tend to have a smaller supply as immigrants tend to be healthier and less likely to donate for cultural reasons.6 Therefore, where one lives made a difference in one’s chance of receiving an organ.
Furthermore, one’s socioeconomic status made a difference because those of lower socioeconomic status were less likely to have access to organs or be able to afford post-transplant care. This is because a person who is living in a region with lower supply has a much higher chance of getting a transplant by moving into a region with a higher supply, and people of lower socioeconomic status often cannot afford to make the move or pay out-of-pocket as Medicaid will not cover organ transplants in another state.7 For example, one Medicaid patient in region 11 was given a quote for $565,000 out-of-pocket for a liver transplant.7 Finally, even after receiving a transplant, patients on Medicaid are often left picking up the tab on immunosuppressant medications to ensure the body won’t reject the organ because the government insurance coverage is not enough.8 Moreover, some of the widely used medications have not officially been approved by the Food and Drug Administration (FDA) and, therefore, are not covered by government insurance.9
In 2018, the rules changed to address the inequities. Lungs will now go to the sickest patients who are a match for the organ within 250 nautical miles of where the donor dies, and hearts will go to the sickest match within 500 nautical miles. This system moves away from the regional system.10 While this policy seemed to make the most sense, there has been a great deal of pushback. Washington University and centers in Georgia, Michigan, Kansas and others have filed a lawsuit against the decision-making body, the United Network for Organ Sharing. They argue that these new rules will heavily favor metropolitan areas where there is greater need and disadvantage rural areas where access to care is less along with higher rates of poverty. Washington University is using their six-month study which finds that after the nationwide policies were implemented, the number of lung transplants remained steady but the costs per person doubled as the retrieval, fees for transportation, and fees for larger teams increased.11 As a result, lawmakers in the state of Kansas introduced a state bill that would allow Kansas organ donors to specify whether they would like their organs to go to somebody in the state.12
The debate around the issue of organ shortage will be ongoing and contentious as policies are established and adjusted in efforts to increase the supply of organs and ensure equitable organ allocation. Hopefully one day, our nation will arrive at policies that result in equitable distribution of this limited resource and reasonable match between supply and demand so that more people can get a second chance at life regardless of their race, location, or socioeconomic status.
Author bio:
.jpg)
Priya Vedula is a health policy analyst at the Institute for Health Policy and Leadership. Her work involves examining health policies and regulations with a focus on oral health, mental/behavioral health, and hunger. She received her Master of Public Health degree from Columbia University.
References:
- https://www.organdonor.gov/statistics-stories/statistics.html
- https://unos.org/community/regions/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3145429/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5382421/
- https://www.jstor.org/stable/10.1086/661256?seq=1#page_scan_tab_contents
- https://journalofethics.ama-assn.org/article/immigrants-and-organ-sharing-one-way-street/2008-04
- https://newrepublic.com/article/145682/gross-inequality-organ-transplants-america
- https://khn.org/news/no-cash-no-heart-transplant-centers-require-proof-of-payment/
- https://www.nytimes.com/2019/04/02/health/organ-transplant-drugs-medicare.html
- https://www.modernhealthcare.com/article/20181207/NEWS/181209931/u-s-organ-transplant-rules-get-an-overhaul
- https://www.stltoday.com/lifestyles/health-med-fit/st-louis-transplant-surgeons-fear-new-organ-allocation-rules-could/article_ee9ef5c2-dc3a-50ed-aaf4-d3a49559d3ef.html#1
